Abstract

Background
It remains uncertain if patients with atrial fibrillation or mechanical heart valves requiring interruption of warfarin for procedures benefit from post-procedure anticoagulant bridging therapy.
Methods
In order to determine the efficacy and safety of postoperative LMWH bridging, we conducted a multicenter randomized double-blind controlled trial of patients with atrial fibrillation or a mechanical heart valve who require interruption of warfarin for a planned procedure. We excluded patients with active bleeding within 30 days, platelet count <100 x10⁹/L, spinal, cardiac or neurosurgery, life expectancy <3months, creatinine clearance <30ml/min, multiple mechanical valves or a Starr-Edwards valve, mechanical valve with history of stroke or TIA, or a history of heparin induced thrombocytopenia. The last dose of warfarin was given 6 days prior to the procedure. All patients received pre-procedure bridging therapy with dalteparin 200 IU per kilogram (max 18,000 IU) subcutaneously in the morning day-3 and day-2 then dalteparin 100 IU per kilogram (max 18,000 IU) subcutaneously 24 hours pre-procedure. Warfarin was resumed in the evening of the procedure at twice the usual dose for the first two days and then titrated according to INR. After the procedure (same day or next day), when hemostasis had been achieved, patients were randomized to receive dalteparin or placebo for at least 4 days and until the INR was greater than 1.9. Randomization was stratified by presence of a mechanical valve, by the post-procedure risk for major bleeding, and by centre. For patients at high risk for post-procedure major bleeding, dalteparin or placebo was administered at a fixed daily dose of 5000 IU. For patients at low risk for post-procedure major bleeding, dalteparin or placebo was administered at a daily dose of 200 IU per kilogram (max 18,000 IU). The primary analysis was a comparison of the proportion of patients who had major thromboembolism (stroke, proximal DVT, PE, MI, peripheral embolism) over 90 days by Chi-squared test according to the intention to treat principle. Secondary outcomes were major bleeding, all cause mortality and a composite outcome of major thromboembolism and major bleeding.
Results
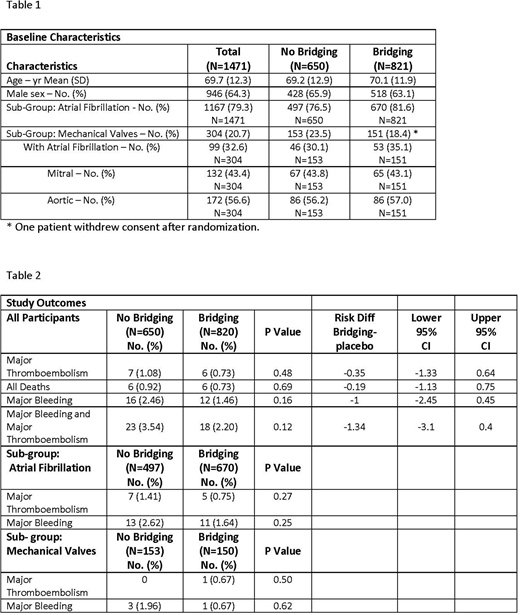
Starting in October 2006 we randomized a total of 1471 patients of whom 1167 had atrial fibrillation (without mechanical heart valves) and 304 had mechanical valves (99 also had atrial fibrillation). Last follow up was completed in May 2016. Baseline characteristics were similar between the LMWH and the placebo groups (see Table 1). Due to a randomization program system error at two centres more atrial fibrillation patients were randomized to dalteparin rather than to placebo. Major thromboembolism occurred in 6/820 (0.71%) dalteparin patients and 7/650 (1.11%) placebo patients. Major post-procedure bleeding occurred in 12 (1.46%) dalteparin patients and 16 (2.46%) placebo patients. Findings were similar in patients with atrial fibrillation alone and in patients with mechanical heart valves (with or without atrial fibrillation) (Table 2).
Conclusions
In patients with atrial fibrillation and/or mechanical heart valves who had warfarin interrupted for a procedure there was no benefit from post-procedure LMWH bridging.
Kovacs:Bayer: Research Funding; Daiichi Sankyo Pharma Development: Research Funding. Wells:Janssen: Honoraria; Sanofi: Honoraria; BMS: Honoraria, Research Funding; Bayer: Honoraria. Schulman:Boehringer-Ingelheim: Honoraria, Research Funding; Daiichi-Sankyo: Honoraria; Sanofi: Honoraria; Bayer: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal